The 4 stages of diabetic retinopathy
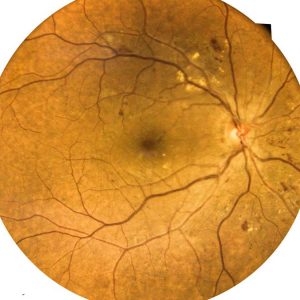
Diabetic retinopathy is a diabetes complication that is caused by damage to the blood vessels of light-sensitive tissue in the back of the retina. It does not always have symptoms in the beginning, or the symptom could be as minor as slight vision problems. There are four stages of diabetic retinopathy.
Stage 1: Mild non-proliferative
This stage involves little to no symptoms. The blood vessels in the retina weaken, and small areas of swelling begin in the retina’s tiny vessels. Tiny bulges called micro aneurysms may form in the blood vessels, causing fluid to leak. The leakage may lead to swelling of the macula.
Stage 2: Moderate non-proliferative
As stage two begins, blood vessels that nourish the retina become blocked and swell. This can lead to diabetic macular edema, which is build up of more fluid in the retina.
Stage 3: Severe non-proliferative
As the disease progresses, more blood vessels are blocked, which disrupts the blood supply. The damaged retina signals the body to produce new blood vessels. Scar tissue may form, causing retinal detachment. Retinal detachment can cause severe vision loss.
Stage 4: Proliferative
During this advanced stage, the retina signals a trigger development of new blood vessels that proliferate in the retina and the vitreous. The vitreous is a transparent gel that fills the interior of the eye. Because the new blood vessels are abnormal, they can rupture and bleed, causing hemorrhages. Scar tissue can develop and and tug at the retina, creating further damage or retinal detachment.
Symptoms of diabetic retinopathy can include blurry vision, flashing lights, cloud or streaks of red in vision, or blind spots. If you have diabetes, you should be aware of retinopathy and how quickly it can develop. The longer a person has diabetes, the higher they are at risk of developing diabetic retinopathy.
